A cikk orvosi szakértője
Új kiadványok
Koronária keringés
Utolsó ellenőrzés: 29.06.2025

Minden iLive-tartalmat orvosi szempontból felülvizsgáltak vagy tényszerűen ellenőriznek, hogy a lehető legtöbb tényszerű pontosságot biztosítsák.
Szigorú beszerzési iránymutatásunk van, és csak a jó hírű média oldalakhoz, az akadémiai kutatóintézetekhez és, ha lehetséges, orvosilag felülvizsgált tanulmányokhoz kapcsolódik. Ne feledje, hogy a zárójelben ([1], [2] stb.) Szereplő számok ezekre a tanulmányokra kattintható linkek.
Ha úgy érzi, hogy a tartalom bármely pontatlan, elavult vagy más módon megkérdőjelezhető, jelölje ki, és nyomja meg a Ctrl + Enter billentyűt.
A koszorúér-keringés (vagy koszorúér-keringés) az érrendszer, amely vérrel és oxigénnel látja el a szív izmait, az úgynevezett szívizomot. A szívizom a szívizomszövet, amely a szív falát alkotja, és lehetővé teszi az összehúzódást és a vér pumpálását az egész testbe.
A koszorúerek, más néven koszorúerek, felelősek a szívizom vérellátásáért. A szív felszínén és a szöveteiben helyezkednek el.
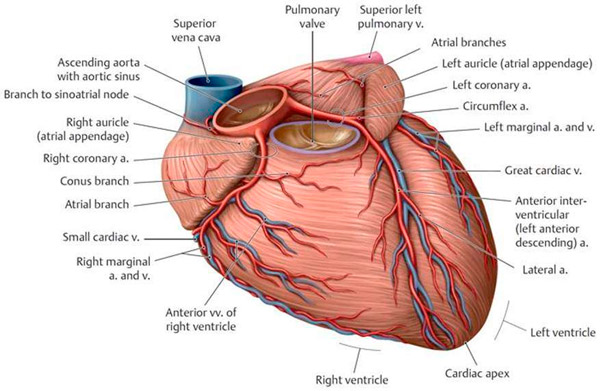
Koszorúerek
Ezek azok az erek, amelyek vérrel látják el a szívizomzatot (szívizomzat). A koszorúerek a szív felszínén és belsejében helyezkednek el, és fontos szerepet játszanak a szívizom oxigénnel és tápanyagokkal való ellátásában, amelyekre a megfelelő működéshez szüksége van. A főbb koszorúerek az alábbiakban soroljuk fel:
Bal koszorúér (LCA):
- Bal elülső leszálló artéria (LAD): A LAD ezen ága a szív elülső oldalán fut, és vérellátást biztosít az elülső és felső szívizomnak.
- Bal oldali circumflex artéria (LCx): Az LCx az LCA-ból ered, és a szívizom hátsó, valamint bal laterális oldalának vérellátását biztosítja.
Jobb koszorúér (RCA):
- A jobb koszorúér az aorta jobb oldalán kezdődik, és vérellátást biztosít a szívizom jobb oldalának és a szív hátsó részének.
Ezek a koszorúerek elágaznak, és kis erek és artériák hálózatát alkotják, amelyek áthatolnak a szívizomon, és oxigénnel és tápanyagokkal látják el annak sejtjeit. A koszorúerek kritikus fontosságúak a normális szívműködéshez, és elzáródásaik vagy szűk keresztmetszeteik szívproblémákat okozhatnak, beleértve az anginát (mellkasi fájdalom) és a miokardiális infarktust (a szívizom egy részének elhalása).
Koszorúerek
Ez egy vénákból álló hálózat, amely felelős a szívizomból (szívizomból) származó salakvér összegyűjtéséért és a szív jobb pitvarába történő elvezetéséért. Fontos szerepet játszanak a vérkeringésben, és oxigénnel és tápanyagokkal látják el a szívet.
A fő koszorúerek a következők:
- Nagy szívvéna: Ez a véna a szív bal kamrájának elülső falán fut, és a szívizom elülső részéből gyűjti össze a vért.
- Kis szívvéna: Ez gyűjti a vért a jobb alsó kamrából, a jobb felső kamrából és a jobb felső pitvarból.
- Középső szívvéna: Ez a szív hátsó falán fut, és a szívizom hátsó részéből gyűjti össze a vért.
A koszorúerek a szívben egyesülve koszorúér-sinust alkotnak, amely a jobb pitvarba ömlik. Fontos, hogy ezek a vénák biztosítsák a salakanyag hatékony összegyűjtését és elvezetését, mivel a koszorúerek megfelelő működése nemcsak oxigént biztosít a szívnek, hanem eltávolítja az anyagcsere-termékeket és a salakanyagokat is, amelyek a szívizomban keletkeznek a munkája során.
A koszorúér-betegség és a koszorúér-betegség súlyos szívproblémákhoz, például koszorúér-betegséghez (CHD), anginához és miokardiális infarktushoz vezethet. Ezek az állapotok orvosi beavatkozást igényelhetnek, beleértve az angioplasztikát és a koszorúér-bypass műtétet, a szív normális véráramlásának helyreállítása érdekében.
A koszorúerek funkciói
A koszorúerek, más néven koszorúerek, fontos funkciókat látnak el a szervezetben, amelyek a szívizom (szívizom) vér- és oxigénellátásával kapcsolatosak. Íme a koszorúerek főbb funkciói:
- Oxigén- és tápanyagszállítás: A koszorúerek felelősek az oxigén és a tápanyagok szívizomba (szívizom) juttatásáért. A szívizomnak folyamatos oxigén- és energiaellátásra van szüksége ahhoz, hogy elvégezze az összehúzódás és a vér pumpálásának feladatát a testben.
- Véráramlás szabályozása: A koszorúerek képesek a szívizom igényeinek megfelelően kitágulni és összehúzódni. A véráramlásnak ez a szabályozása lehetővé teszi, hogy az oxigén- és tápanyagellátás a szív aktivitási szintjéhez igazodjon.
- A megfelelő szívműködés biztosítása: A koszorúerek megfelelő vérellátást biztosítanak a szívnek, beleértve a saját szívizomsejtjeit is, így a szív hatékonyan össze tud húzódni és fenntartani a véráramlást.
- Érelmeszesedés elleni védelem: Az egészséges koszorúerek képesek megakadályozni az érelmeszesedés (koleszterin és más anyagok felhalmozódása az artériák falán) kialakulását. Azonban áldozatul eshetnek az érelmeszesedéses folyamatoknak, amelyek koszorúér-elzáródáshoz és koszorúér-betegséghez vezethetnek.
A koszorúerek kritikus fontosságúak a szív- és érrendszer egészsége és működése szempontjából. Működésük bármilyen károsodása, például a szűkület (szűkület) vagy az elzáródás, súlyos szívproblémákhoz vezethet, beleértve az angina pectorist, a miokardiális infarktust és a szívelégtelenséget. Ezért fontos az egészséges koszorúerek fenntartása, az egészséges életmód követése és a kockázati tényezők, például a magas vérnyomás és a koleszterinszint szabályozása.
A koszorúér véráramlása kritikus fontosságú a normális szívműködéshez. Amikor a szív összehúzódik, elegendő oxigénre és tápanyagra van szüksége, amelyeket a koszorúereken keresztül juttatnak be. Ha a koszorúerek beszűkülnek vagy elzáródnak, az miokardiális ischaemiához (vérellátás hiányához) vezethet, ami anginát (mellkasi fájdalmat) vagy miokardiális infarktust (a szívizom egy részének elhalását) okozhat.
A koszorúér-keringés élettana
Magában foglalja azokat a folyamatokat, amelyek biztosítják a szívizom (szívizom) normális vérellátását. A szívizomban a véráramlás némileg eltér a test más szerveinek és szöveteinek véráramlásától speciális funkciója és magas energiaigénye miatt. Íme a legfontosabb szempontok:
- Autoreguláció: A koszorúerek autoregulációs mechanizmusokkal rendelkeznek, amelyek lehetővé teszik számukra, hogy automatikusan módosítsák átmérőjüket és véráramlásukat a szívizom oxigén- és tápanyagigényének változásaihoz igazodva. Amikor a szívizomnak több vérellátásra van szüksége, az artériák kitágulnak, több vért és oxigént biztosítva. Nyugalmi állapotban az artériák szűkülhetnek.
- Diasztolés periódus: A szívizom fő vérellátása a szívciklus diasztolés fázisában történik, amikor a szív ellazult, és a üregek megtelnek vérrel. Ezen a ponton az artériák több vért és oxigént tudnak fogadni, mivel a szívizom nem nyomja őket össze.
- Arteriovenózus anasztomózisok: Az arteriovenózus anasztomózisok a szívizomban találhatók, amelyek az artériák és a vénák közötti összeköttetést biztosítják. Vértartályként szolgálhatnak, és további vérellátást biztosíthatnak a szív fokozott terhelése esetén.
- Vegetatív idegrendszer: A szimpatikus aktiváció (a stresszválasz aktiválódása) növelheti a szívizom véráramlását, növelve a perctérfogatot és tágítva a koszorúereket. Erős szimpatikus aktiváció esetén azonban a koszorúerek szűkülhetnek is.
- Endothelium és nitrogén-monoxid: A koszorúerek endotéliuma (az érfal belső rétege) nitrogén-monoxidot termel, amely segít az artériák tágításában és a szívizom normális vérellátásának fenntartásában.
Ezek a fiziológiai mechanizmusok lehetővé teszik, hogy a szív elegendő oxigént és tápanyagot kapjon a tevékenység és a nyugalmi állapot különböző időpontjaiban, biztosítva, hogy hatékonyan működjön a szervezet vérpumpájaként.
A koszorúér-keringés szabályozása
Több fiziológiai és biokémiai mechanizmus összehangolásával működik, hogy biztosítsa a szívizom (szívizom) megfelelő vérellátását különböző körülmények között. A főbb szabályozó mechanizmusok a következők:
- Autoreguláció: A koszorúerek képesek automatikusan módosítani az átmérőjüket a vérnyomás és a szívizom igényeinek változásaihoz igazodva. Amikor a szívizomnak több vérellátásra van szüksége, az artériák kitágulnak, hogy további véráramlást biztosítsanak.
- Anyagcsere-szabályozás: Amikor a szívizom aktívabb, például testmozgás közben, az anyagcsere-termékek, például az adenozin és az acilkoffein szintje megemelkedik a szívizomban. Ezek a termékek tágíthatják a koszorúereket, növelve a véráramlást ott, ahol arra a legnagyobb szükség van.
- Szimpatikus idegrendszer: A szimpatikus idegrendszer stimulálása a koszorúerek összehúzódását vagy tágulását okozhatja. A szimpatikus aktiváció, például stresszre vagy fizikai aktivitásra adott válaszként, növelheti a szívizom véráramlását a koszorúerek tágításával.
- Vérlemezke-adhézió és -koaguláció: Koszorúér-sérülés esetén a vérlemezke-adhéziós és -koagulációs mechanizmusok aktiválódhatnak a vérzés megelőzése és az érfal integritásának helyreállítása érdekében.
- Endothelium és nitrogén-monoxid: A koszorúerek endotéliuma (az érfal belső rétege) nitrogén-monoxidot termel, amely egy olyan molekula, amely segít kitágítani az ereket és csökkenteni azok összehúzódását.
Ezek a mechanizmusok szorosan együttműködnek a szívizom normális vérellátásának fenntartása érdekében különböző körülmények között. A koszorúér véráramlását szabályozzák, hogy biztosítsák a szívizom megfelelő vérellátását és fenntartsák annak teljesítményét.
Koszorúér-keringési zavar
A koszorúér-betegség, más néven koszorúér-betegség (CAD) vagy koszorúér-betegség (CHD), akkor fordul elő, amikor a szívizom (szívizom) megfelelő oxigén- és tápanyagellátása korlátozott vagy megszakad a koszorúerek problémái miatt. Ez számos súlyos tünetet és szövődményt okozhat. Az alábbiakban a koszorúér-keringési zavarok néhány főbb aspektusát ismertetjük:
- Angina (stabil és instabil): Az angina mellkasi fájdalom, amely általában testmozgás vagy stressz hatására jelentkezik, és nyugalmi állapotban vagy nitroglicerin bevétele után javul. A stabil angina általában valamilyen aktivitás során jelentkezik, és természeténél fogva kiszámítható, míg az instabil angina nyugalmi állapotban is előfordulhat, és gyakran a koszorúér-keringés súlyosabb problémájára utal.
- Miokardiális infarktus: Miokardiális infarktus (szívroham) akkor következik be, amikor az egyik koszorúér teljesen elzáródik, és a szívizom egy részének vérellátása megszűnik. Ez egy rendkívül súlyos állapot, amely azonnali orvosi ellátást igényel.
- Fájdalom nélküli angina (néma szívroham): Egyes embereknél jelentős mellkasi fájdalom nélkül is előfordulhat miokardiális infarktus. Ehelyett rossz közérzetet, fáradtságot, hátfájást, nyakfájást, állkapocsfájdalmat vagy gyomorfájást tapasztalhatnak.
- Krónikus koszorúér-betegség: Ezt az állapotot a koszorúér-véráramlás krónikus károsodása jellemzi, ami tartós tüneteket okozhat, mint például fáradtság, légszomj és mellkasi fájdalom.
- Szívritmuszavarok és szívritmuszavarok: A szív oxigénhiánya aritmiákat és szívritmuszavarokat okozhat, amelyek életveszélyesek lehetnek.
- Szívelégtelenség: A koszorúér-keringés tartós károsodása a szívműködés romlásához és szívelégtelenség kialakulásához vezethet.
A koszorúér-betegség kezelése a probléma kiterjedésétől és súlyosságától függ. Ez magában foglalhatja a gyógyszeres terápiát, az angioplasztikát és a koszorúér-bypass műtétet, valamint az életmódbeli változásokat, beleértve az étrendet és a testmozgást. A rendszeres orvosi ellenőrzés és az orvos ajánlásainak betartása fontos szerepet játszik a koszorúér-betegség kezelésében.
Koszorúér-keringési zavar az EKG-n
Az elektrokardiogramon (EKG) többféleképpen is megjelenhet, és a jellemző változások attól függenek, hogy a szívizom (szívizom) mely részei voltak ischaemiának (elégtelen vérellátásnak) kitéve. Íme néhány tipikus EKG-elváltozás, amelyek a koszorúér-véráramlás károsodására utalhatnak:
- ST-szakasz:
- ST-szakasz emelkedés: A koszorúér-betegség egyik legjellemzőbb jele az EKG-n látható ST-szakasz emelkedés. Ez akut koszorúér-eseményre, például miokardiális infarktusra utalhat.
- ST-szakasz depresszió: Alkalmanként az ST-szakasz depressziójának változásai is megfigyelhetők, ami szintén az iszkémia indikátora lehet.
- A T változásai: Az EKG-n a T-karmok alakjának és amplitúdójának változásai mutatkozhatnak, ami a koszorúér-véráramlás zavarára utalhat.
- ST-szakasz depresszió: Az ST-szakasz szintjének az alapvonal alá esése az iszkémia jele lehet, különösen testmozgás vagy stressz esetén.
- Tünetmentes változások: Egyes betegeknél EKG-elváltozások jelentkezhetnek, amelyeket nem kísérnek tünetek. Ezek az elváltozások rendszeres fizikális vizsgálat vagy monitorozás során észlelhetők.
- Változások a vezető ritmusban: A koszorúér-keringési zavar a szív vezető ritmusát is befolyásolhatja, ami aritmiákhoz vagy elzáródásokhoz vezethet.
Fontos felismerni, hogy az EKG-elváltozások önmagukban nem mindig jelentenek egyértelmű diagnózist. A pontos diagnózis felállításához és a koszorúér-betegség súlyosságának meghatározásához gyakran további vizsgálatokra, többek között angiográfiára (a koszorúerek kontrasztanyagos röntgenvizsgálata) és egyéb technikákra van szükség. Ha koszorúér-betegséggel összefüggő tünetei vannak, vagy ha az EKG rendellenességeket mutat, mindenképpen konzultáljon orvosával további kivizsgálás és a legjobb kezelés meghatározása érdekében.
Akut koszorúér-betegség
Ez egy olyan állapot, amelyben a szívizom (szívizom) oxigén- és tápanyagellátása akut és elégtelen a koszorúerek elzáródása miatt. Ez az állapot általában a koszorúerekben kialakuló érelmeszesedésnek (koleszterin és más anyagok felhalmozódásának az artériákban) vagy trombózisnak (vérrögképződésnek) köszönhető. Az akut koszorúér-betegség többféle formát ölthet:
- Instabil angina (instabil angina): Ez egy olyan állapot, amelyben a szívizom vérellátása átmenetileg károsodik, általában vérrögképződés vagy a koszorúerek szűkülete miatt. Ez súlyos mellkasi fájdalmat okozhat, amely általában nyugalmi állapotban nem múlik el, és más tünetekkel is járhat, például légszomjjal és eszméletvesztéssel.
- Miokardiális infarktus (szívroham): Ez egy súlyosabb állapot, amelyben a szívizom vérellátása teljesen vagy részlegesen megszűnik, ami a szívizom egy részének elhalásához vezet. A tünetek közé tartozik a súlyos mellkasi fájdalom, a bal karba, nyakba vagy hátra kisugárzó fájdalom, légszomj, hányinger és hányás.
- Akut koszorúér-elzáródás szindróma miokardiális infarktus nélkül (instabil angina infarktus nélkül): Ez egy olyan állapot, amelyben a koszorúér akut elzáródása van, de a miokardiális szövetek elhalása még nem következett be. A tünetek hasonlóak lehetnek az instabil anginához, de súlyosabbak.
Bármely akut koszorúér-vérzési rendellenesség sürgős orvosi ellátást igényel. A kezelés magában foglalhatja a vérhígításra és a koszorúerek tágítására szolgáló gyógyszerek alkalmazását, angioplasztikai beavatkozásokat (a beszűkült artériák kitágítása) vagy koszorúér-bypass műtétet. A gyors orvosi ellátás és az időben történő kezelés elengedhetetlen a súlyos szövődmények megelőzése és a miokardiális infarktus kockázatának csökkentése érdekében.
Koszorúér-keringési elégtelenség kezelése
A koszorúér-betegség (koszorúér-betegség) kezelése számos gyógyszeres és nem gyógyszeres módszert foglalhat magában. A kezelés célja a tünetek csökkentése, az életminőség javítása és a szövődmények megelőzése. Íme néhány a koszorúér-betegség kezelésére alkalmazható gyógymódok és módszerek közül:
- Vérnyomáscsökkentő gyógyszerek:
- Béta-adrenoblokkolók: Csökkentik a pulzusszámot és a szív terhelését.
- Kalcium antagonisták: Segíthetnek a koszorúerek tágításában és a szív összehúzódási képességének csökkentésében.
- Angiotenzin-konvertáló enzim inhibitorok (ACE-gátlók) és angiotenzin receptor antagonisták (ARB-k): Javítják a véráramlást és csökkenthetik a szív terhelését.
- Nitrátok: Az értágítók, mint például a nitroglicerin, segíthetnek a koszorúerek tágításában és a szívizom vérellátásának javításában. Ezeket az anginás rohamok enyhítésére használják.
- Antitrombotikus terápia: Az olyan gyógyszerek, mint az acetilszalicilsav (aszpirin) és az antikoagulánsok segíthetnek megelőzni a vérrögök kialakulását a koszorúerekben.
- Koleszterinszint csökkentése: A sztatin gyógyszereket a "rossz" koleszterin (LDL) csökkentésére és az érelmeszesedés megelőzésére használják.
- Cukorbetegség kezelésére szolgáló gyógyszerek: Cukorbetegség esetén a vércukorszintet szigorúan ellenőrizni kell.
- Életmódbeli ajánlások: Tartalmazzon alacsony sótartalmú és zsírtartalmú étrendet, testmozgást, dohányzásról való leszokást és stresszkezelést.
- Rehabilitáció miokardiális infarktus után: A rehabilitációs programok segíthetnek a betegeknek visszanyerni a fizikai aktivitást, kontrollálni a kockázati tényezőket és erősíteni a szívet.
- Intervenciós eljárások: Ez magában foglalhatja az angioplasztikát (a beszűkült koszorúerek kiszélesítése ballonnal) vagy a koszorúér-bypass műtétet (új erek beültetése a beszűkült artériák területeinek megkerülésére).
A koszorúér-elégtelenség kezelését az orvosnak kell egyénre szabnia, az egyes betegek klinikai jellemzői alapján. Fontos, hogy betartsuk az orvos ajánlásait, és rendszeres orvosi ellenőrzéseken vegyünk részt a szív állapotának ellenőrzése és a szövődmények megelőzése érdekében.

